Find Dry Needling Near Me
Introduction to Dry Needling
Dry needling is a modern treatment that is becoming increasingly popular for managing muscle pain and improving mobility. It has been argued that dry needling is actually a branch of acupuncture, debated between Traditional Chinese Medicine Doctors and physical therapists. In America, dry needling and acupuncture are categorized into different modalities. This article will guide you through what dry needling is, who can perform it, its benefits, and how you can find the best practitioners near you.
What is Dry Needling?
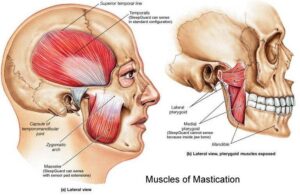
Dry needling involves inserting a thin needle into the muscle’s trigger points. It is not acupuncture, but rather a physical therapy aimed at easing muscular and myofascial pain and cramps. Dry needling, combined with electrical currents from a transcutaneous electrical nerve stimulation (TENS) machine, can further stimulate the targeted acupoints or trigger points to enhance the treatment effects.
Benefits of Dry Needling
The technique offers several benefits:
- Reduces pain and soreness
- Releases myofascial trigger points
- Enhances joint range of movement
- Speeds up recovery from injuries
- Decreases muscle tension
Conditions That Can Be Helped or Managed
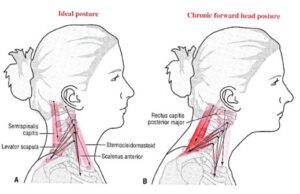
- Neck pain, including torticollis
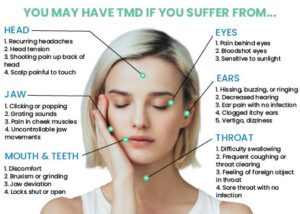
- TMJ pain and TMJ headaches
- Shoulder pain, including subacromial and subdeltoid bursitis
- Back pain, including sciatica and herniated discs
- Knee pain, including meniscus tears and bursitis
- Leg pain, including shin splints
- Whiplash injuries
- Sports injuries, including muscle strains and sprains
- Chronic pain disorders, managing fibromyalgia and myofascial pain syndrome
- Headaches and migraines
- Arthritis, managing associated muscle pain
- Tendinitis, including tennis elbow, golfer’s elbow, and plantar fasciitis
Who Can Perform Dry Needling?
Apart from registered acupuncturists and Traditional Chinese Medicine Doctors, allied health practitioners such as chiropractors, physiotherapists, and remedial massage therapists who have completed dry needling courses can perform dry needling.
How to Find Dry Needling Services
Finding the right dry needling service involves a few steps:
Search Engines and Online Directories
Simply typing “dry needling near me” into Google or Bing can help you find the closest clinics near you with previous patients’ star reviews and comments, providing insight. Alternatively, checking online directories lists qualified practitioners by location.
Recommendations from Local Healthcare Providers or Fitness and Wellness Centers
Your general practitioners (GP) or physical therapists often have a network of trusted allied health providers. Likewise, local gyms and wellness centers sometimes know who offers the best dry needling services from their personal experience.
Word of Mouth
Word of mouth is always the best for referrals because the best dry needling providers are recommended without any commercial purposes.
Consultation Before Treatment
A good practitioner will always offer a consultation to discuss your needs, explain the process, and what you can expect after dry needling.
What to Expect During a Session
The Process
The practitioner will identify trigger points and insert needles to release tension and pain. Mild discomfort is expected during dry needling. Dry needling with electro-stimulation may be used to achieve a better result, depending on the judgment of the healthcare practitioner. The needles stay in place for roughly 10-15 minutes to maximize the effects.
Aftercare Tips
Follow these tips to maximize the benefits of your session and ensure a quick recovery:
- Rest – Avoid any strenuous activities or exercise immediately after treatment. Resting allows your body to recover after needling.
- Hydration – Keeping hydrated can aid in muscle recovery.
- Heat Application – A heat pad can accelerate blood flow and reduce residual soreness.
- Stretching – This maintains the benefits of the treatment and increases flexibility.
- Monitor for Bruising or Discomfort – Mild swelling, bruising, or discomfort can occur after needling. Normally, these subside within a few days.
- Follow-Up Treatments – Multiple treatment sessions may be needed, depending on your condition.
Looking for dry needling near me?
Kings Park Chiropractic Clinic provides dry needling services, you can book your appointment via online booking system or contact us by 9837 5161.



 Chiropractic care, a popular alternative medicine, is celebrated for its effectiveness in alleviating pain, enhancing mobility, and boosting overall well-being without resorting to surgery or drugs. Central to chiropractic treatment is the chiropractic adjustment, which often raises questions and concerns, especially among newcomers. A common inquiry is: Does undergoing a chiropractic adjustment cause pain?
Chiropractic care, a popular alternative medicine, is celebrated for its effectiveness in alleviating pain, enhancing mobility, and boosting overall well-being without resorting to surgery or drugs. Central to chiropractic treatment is the chiropractic adjustment, which often raises questions and concerns, especially among newcomers. A common inquiry is: Does undergoing a chiropractic adjustment cause pain?