Family is the cornerstone of our lives, and ensuring the well-being of every family member is of utmost importance. At Kings Park Chiropractic, we offer specialized family chiropractic care to enhance the health and well-being of each family member, from children to adults and seniors. Led by Dr. Brian Sin, our experienced team is dedicated to providing comprehensive and personalized care that addresses the unique needs of every individual.
Meet Dr. Brian Sin: Your Trusted Family Chiropractor:
Dr. Brian Sin is a trusted family chiropractor who has been serving the Kings Park community for years. His passion for chiropractic care and his commitment to patient-centered treatments make him the ideal choice for your family’s well-being. Dr. Sin understands the specific needs of each family member and creates tailored treatment plans to ensure the best possible outcomes.
Understanding the Importance of Family Chiropractic Care:
Family chiropractic care focuses on optimizing spinal health and function for individuals of all ages. It recognizes that each family member has unique needs and tailors the care accordingly. By addressing spinal misalignments, improving joint mobility, and supporting overall wellness, family chiropractic care promotes better health and quality of life for the entire family.
Benefits of Family Chiropractic Care:
Family chiropractic care offers numerous benefits for each family member:
Improved Spinal Health and Function:
Chiropractic adjustments help restore proper alignment and function of the spine, reducing nerve interference and promoting optimal nervous system function. This leads to improved spinal health, better communication between the brain and the body, and enhanced overall well-being.
Enhanced Overall Well-being:
Chiropractic care is not just about addressing pain or discomfort; it is about promoting holistic well-being. By improving spinal health, chiropractic care positively influences various aspects of health, including immune function, sleep quality, digestion, and energy levels.
Specialized Chiropractic Services for Each Family Member:
At Kings Park Chiropractic, we provide specialized chiropractic services to meet the unique needs of each family member.
Chiropractic Care for Children and Adolescents:
Children and adolescents can benefit greatly from chiropractic care. As their bodies grow and develop, proper spinal alignment plays a crucial role in their overall health and well-being. Chiropractic care for children focuses on supporting healthy growth, addressing postural issues, and detecting and correcting spinal misalignments at an early age.
Gentle Chiropractic Techniques for Children:
Chiropractic adjustments for children utilize gentle and safe techniques that are appropriate for their developing bodies. These techniques aim to correct spinal misalignments, improve nervous system function, and support optimal growth and development.
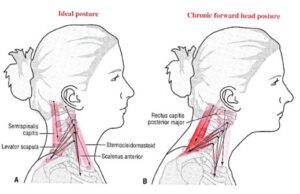
Addressing Postural Issues and Spinal Misalignments:
Children and adolescents often face postural challenges due to prolonged sitting, carrying heavy backpacks, or engaging in sports activities. Chiropractic care can help address these postural issues and correct spinal misalignments, reducing the risk of future health problems.
Chiropractic Care for Adults:
Adults can also benefit greatly from chiropractic care. Whether you are experiencing back pain, headaches, or other musculoskeletal issues, chiropractic care can provide effective relief and improve your overall health and well-being.
Relieving Pain and Discomfort:

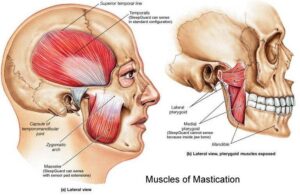
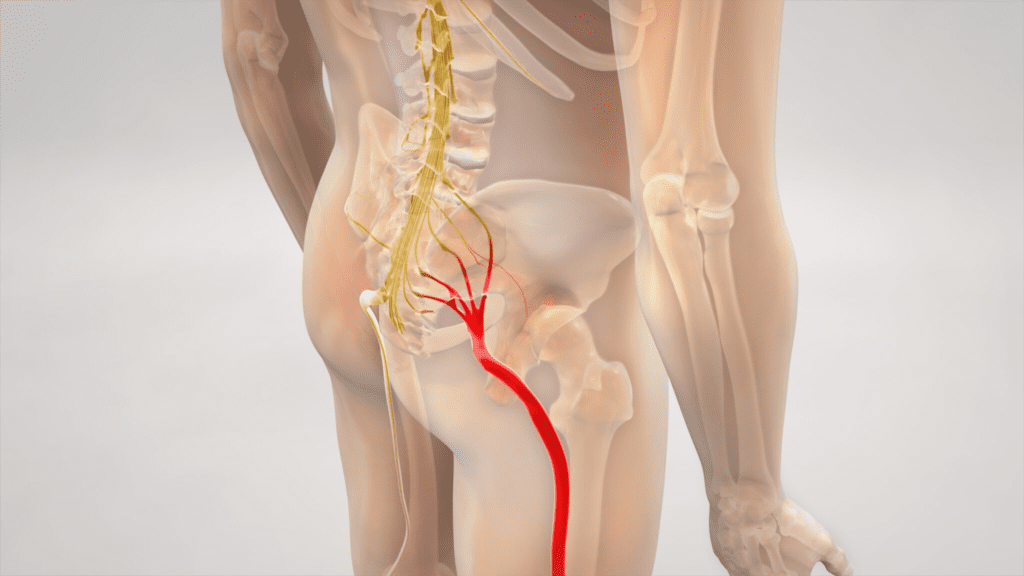
Chiropractic adjustments help alleviate pain and discomfort by addressing the underlying causes of your symptoms. Whether it’s back pain, neck pain, joint pain, or headaches, chiropractic care aims to restore proper alignment, reduce inflammation, and promote natural healing.
Treating Common Conditions like Back Pain and Headaches:
Back pain and headaches are common complaints among adults. Chiropractic care offers non-invasive and drug-free solutions to these conditions. By addressing the root cause of the pain, chiropractic adjustments provide long-lasting relief and improve your quality of life.
Restoring Joint Mobility and Function:
Chiropractic care also focuses on improving joint mobility and function. Whether you have restricted range of motion or stiffness in your joints, chiropractic adjustments can help restore proper joint function, allowing you to move more freely and comfortably.
Chiropractic Care for Seniors:
As we age, our bodies undergo changes that can affect our spinal health and overall well-being. Chiropractic care for seniors focuses on promoting healthy aging, enhancing mobility, and improving the quality of life for older adults.
Addressing Age-Related Musculoskeletal Issues:
Seniors often face musculoskeletal issues such as arthritis, osteoporosis, and degenerative disc disease. Chiropractic care offers gentle and effective treatments that aim to alleviate pain, improve joint function, and enhance overall mobility.
Enhancing Balance and Stability:
Chiropractic care also focuses on improving balance and stability in seniors. Through targeted adjustments and exercises, chiropractors can help reduce the risk of falls and improve overall stability, promoting a more active and independent lifestyle.
Comprehensive and Personalized Family Care:
At Kings Park Chiropractic, we provide comprehensive and personalized care for every family member. We understand that each individual has unique needs and goals, and we tailor our treatments accordingly.
Initial Assessment and Examination:
Our team begins by conducting a thorough assessment and examination of each family member. This helps us understand the specific health concerns, past medical history, and goals of every individual. We take the time to listen and address any questions or concerns you may have.
Tailored Treatment Plans for Each Family Member:
Based on the assessment, we develop tailored treatment plans for each family member. These plans may include chiropractic adjustments, therapeutic exercises, lifestyle recommendations, and nutritional guidance. Our goal is to provide individualized care that supports the unique needs of each family member.
Education and Lifestyle Recommendations:
We believe that education is an essential aspect of family chiropractic care. We provide valuable information and guidance on posture, ergonomics, nutrition, exercise, and other lifestyle factors that can enhance the effectiveness of chiropractic care and promote overall well-being.
Choosing Kings Park Chiropractic for Your Family’s Well-being:
When it comes to your family’s well-being, choosing the right chiropractic clinic is essential. At Kings Park Chiropractic, we pride ourselves on our experienced and caring team, state-of-the-art facilities, and convenient location in Kings Park.
Experienced and Caring Team:
Our team is composed of experienced chiropractors who have extensive knowledge and expertise in providing family chiropractic care. We are passionate about helping families achieve optimal health and well-being.
State-of-the-Art Facilities and Equipment:
Our clinic is equipped with state-of-the-art facilities and advanced chiropractic equipment to ensure the highest standard of care for our patients. We create a warm and welcoming environment where you and your family can feel comfortable and at ease.
Convenient Location in Kings Park:
We understand the importance of convenience when it comes to family healthcare. Our clinic is conveniently located in Kings Park, providing easy access to families in the surrounding areas.
Take the First Step Towards Family Wellness: Schedule an Appointment:
If you are ready to prioritize your family’s health and well-being, we invite you to schedule an appointment at Kings Park Chiropractic. Our team is here to support you and provide the exceptional care that your family deserves.